Research article
Apollo hospital, Jubilee hills, Hyderabad, India.
*Corresponding Author: Srinagesh Vadrevu
Citation: Dr. Srinagesh Vadrevu, MS, MCh, Dr. Ramakrishna Pinjala, MS, FRCS Ed, Apollo hospital, Jubilee hills, Hyderabad. A misunderstood and ignored condition – Lipedema, Clinical and Medical Research and Studies. 2(1).
Copyright: © 2023 Ramakrishna Pinjala, This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: January 25, 2023 | Accepted: February 03, 2023 | Published: February 15, 2023
Abstract
Lipedema is a relatively common, unrecognized connective tissue disorder. It affects about 11% of women across the globe. In lipedema, there is symmetrical abnormal deposition of fat especially in the lower extremities. Lipedema can be accompanied with pain, spider veins and easy bruising. Lipedema is rare in men. The disease is progressive in nature. Trigger points for lipedema appear to be puberty, pregnancy and menopause. The disease affects various aspects of the connective tissues like lymphatics, veins, skin, ligaments and even joints as it progresses. Oestrogen and progesterone abnormalities seem to have a role in the progression of the condition. Lipedema also appears to have a genetic predisposition. Lipedema is classified into 4 stages depending on the degree and type of abnormal fat deposition. The severe form can be confused with Dercum’s disease. Depending on the site of deposition of abnormal fat, lipedema is also classified into 5 different types. Lipedema is often confused to be obesity or lymphedema and treated accordingly. Treatments are based on the stages and types of lipedema. Lipedema is extremely difficult to manage with diet, exercises and bariatric surgery alone. All treatments are focused around improving the quality of life, improving physical abilities and appearances.
Keywords: Lipedema; tissue disorder; spider veins; menopause; lymphatics
Introduction
Lipedema is a common, unrecognized connective tissue disorder seen to affect the adipose tissues in the lower extremities and sometimes in the upper extremities as well. It has been estimated that almost 11% of women are affected worldwide[1]. It is seen to affect the buttocks, thighs and legs in the lower extremities sparing the feet more often. It affects the arms and forearms less commonly while sparing the hands. Lipedema is rare in men. Puberty, pregnancy, menopause and stressful conditions trigger the onset of lipedema[2].
Allen and Hines from Mayo clinic USA [3] and Monocorps from Germany [4]gave a detailed description about lipedema in 1940 but still remains to be largely unrecognized. Lipedema has been included in the International Classification of diseases (ICD- 11) of the World Health Organization as a separate clinical entity in the category “Certain noninflammatory disorders of subcutaneous fat,” code EF02.2. According to ICD-11 description, “Lipedema is characterized by non-pitting diffuse “fatty” swelling, usually confined to the legs, thighs, hips and upper arms. It may be confused with lymphedema”[5]. The diagnostic criteria for lipedema were first described in 1951 by Wold etal [6]and have been modified in recent years by Herbst[7]. Lipedema is often associated with comorbidities such as lymphedema, obesity, venous disorders, joint disorders, hormonal fluctuations, and genetic abnormalities.
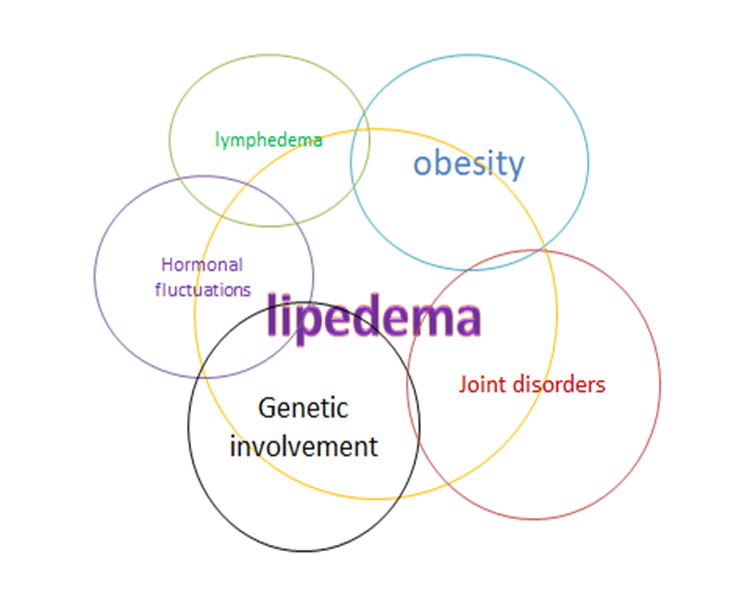
Figure 1: Lipedema and its association with comorbidities
Lipedema and lymphedema
Lipedema is often confused with obesity or lymphedema due to the increased lower body size [8]. Many patients suffering from lipedema are treated for lymphedema due to misconception. Foldi and Foldi (2012) suggest that 15-17% of women being treated for lymphedema have lipedema as well. In late stages of lipedema, lymphatic dysfunction is a frequent finding. However there are many distinct characteristics that differentiate lymphedema from lipedema [9,10,11]. In lipedema patients, the swelling around the ankles in the legs and at the wrist in the upper limb usually stops abruptly giving an ankle cuff and wrist cuff like appearance along with sparing of the feet and hands. Lymphoscintigraphy studies in lipedema have demonstrated microcirculation changes especially in the lymphatic vessels suggesting lymphostasis [12,13,14,15]. There is a loss of elastic recoil of lymphatic vessels in lipedema. This allows more fluid to enter the interstitial space and accumulate between the dermal skin fibers [16,17]. There is an inhibition of lymph flow and leakage of lymphatics and capillaries in gynoid fat [18]. Manual lymphatic drainage as a treatment results in reduction of symptoms and circumference of the limb confirming the existence of the lymphatic component [19]. Idiopathic cyclic edema and cellulite are two aggravating factors associated with edema which are common accompaniments in lipedema [19]. According to a study in the publication phase, 10% have idiopathic cyclic edema and cellulite in more than 50% of women [20]. All these multiple factors are involved in the formation of edema leading to an overload in the lymphatic system. The hallmark of lipedema is a narrow waist, disproportionate adipose tissue deposition in the extremities, more in the lower body, while the hands and feet appear normal [21]. Stemmers’s sign is negative in a typical case of lipedema [22] where the skin over the dorsum of the foot adjacent to 2nd and 3rd toes can be pinched. Lipedema is a progressive disease whose progress is not uniform [9,22,23].

Figure 2: Comparison between lipedema and lymphedema
Lipedema and obesity
Lipedema is different from obesity. However lipedema and obesity can coexist and can be seen in almost 75% of women [24]. Lipedema is characterized by a narrow torso but with an oversized lower body and sometimes the upper limbs. Obesity is characterized by a large midsection and may or may not be accompanied with large limbs. Progressive growth of adipose tissue in the lower body restricts the ability to exercise which could have an effect on weight gain leading to obesity. The adipose tissue under the skin in lipedema could have a rice grain texture and progress to nodular with a “beans in a bag” feel and can be significantly tender to pressure and touch. The main aggravating factor of edema in lipedema is obesity. Kinking of the lymph vessels due to the engulfing surrounding adipose tissue leads to overload and formation of lymphedema. A combination of effective lymphatic drainage techniques and prophylactic weight loss and fat reduction helps avoid aggravation of the condition are some of the best therapeutic approaches. Lipedema, one of the Rare Adipose Disorders (RAD) which includes multiple symmetric lipomatosis (MSL) and Dercum’s disease is often confused with obesity. Standard lifestyle changes like, reduced caloric intake and increased physical activity are effective for obesity and for obesity component of RADs [7]. Lipedema patients in contrast to obese patients have a lower risk to develop diabetes mellitus.

Figure 3: Comparison between lipedema and obesity
Lipedema and joint disorders
Pain in the knee joints and low back due to lordosis and changes in the structure of the spine, tendons and ligaments is not uncommon in lipedema [17]. Hypermobile joints are seen in almost 50% [7] of women suffering from lipedema with features consistent with Ehlers Danlos syndrome. Nearly 41% of women have arthritis of the knee joints [21]. Progressive accumulation of fat in the inner thighs and fat pads around the knees results in a genu valgum and overpronation of the foot resulting in differential erosion and early wear and tear of the joint cartilages. Degeneration of the knee and hip joints may worsen as lipedema progresses [25]. This could lead to early knee joint replacement.

Figure 4: Joint disorders in lipedema
Lipedema and venous disorders
Venous disorders like spider veins or venous telengactasia and varicose veins is seen to be associated with lipedema in almost 39-53% of women [26]. The presence of spider veins in lipedema could be one of the reasons for the aches and heavy feelings of the legs which get worse after sitting or standing for prolonged periods of time. Varicose veins in lipedema need to be addressed depending on various factors like the size in proportion to the limb volume, tortuosity and reflux. Lower limb cellulitis or skin ulceration is more often seen in lymphedema rather than in lipedema unless secondary lipo-lymphedema has developed. Swelling in lymphedema affects the ankles and feet. In lipedema, the swelling is seen in thighs and buttocks rather than in the feet [19].
Lower extremity ultrasound to assess venous competency can be helpful to confirm the diagnosis. If CT or MRI studies are performed as part of initial workup, the absence of circumferential fatty hypertrophy will exclude lipedema as a contributing factor.

Figure 5: Venous problems in lipedema
Lipedema and hormonal fluctuations
The progression of lipedema is slow in some women and rapid in others. This could be due to the relative sensitivity and activity of the hormones, especially oestrogen released in the body. Fat angiogenesis is necessary to maintain adipose tissue health while also promoting growth and expansion [27]. Vascular endothelial growth factors (VEGFs) are a family of secreted proteins which act through receptor kinases to initiate angiogenesis, the branching of new capillaries from an existing vascular bed [28]. Investigation between the relation of estrogen and VEGF reported an upregulation of VEGFA expression with estrogen treatment, indicating the importance of estrogen in VEGF regulation [29,30]. Estrogen, a key regulator of adipocyte lipid and glucose metabolism, and female- associated body fat distribution are postulated to play a contributory role in the pathophysiology of lipedema [31]. Hypothyroidism was found in almost 27-37% of women affected by lipedema [32,33].
Lipedema and genetic abnormalities:
Lipedema is seen to occur in many women in certain families which gives an impression that it is nothing unnatural resulting in acceptance and neglect until late. It has been found that up to 64% of women give a family history of lipedema and hence a genetic history is strongly suggested [7]. Eleven genes related to syndromic lipedema, involved in seven different comorbidities have been identified [34]. The most prominent gene variant found is AKR1C1, a gene that has been involved in progesterone metabolism [35], and is highly expressed in adipocytes and subcutaneous fat [36] in lipedema.
Morphology of lipedema fat:
A comparative study of stem cells derived from normal and lipedema subcutaneous tissue from lateral thigh was done. Lateral adipose tissues revealed a significant increase in the number of cells accompanied by elongated, partly spindle shaped appearance with rounded nuclei at 11-14 days without adipogenic stimuli. However with adipogenic stimuli on days 7 and 14 of culture, the cell morphology changed from having a spindle- like appearance to adipocyte- like shape [37]. Subcutaneous adipose tissue (SAT) from the lower extremities in lipedema patients showed hypertrophic and hyperplastic adipocytes and increased intercellular fibrosis [38,39]. There is report that adipose tissue of lipedema individual undergoes major structural and functional reprogramming [38],including increased unstimulated lipid release [40], tissue inflammation, and excessive fluid accumulation [38,41].
Depending on the amount of abnormal fat accumulation lipedema is classified into 4 stages.
Stages of lipedema
As the disease advances, lipedema involves accumulation of fluid in the fat. Enlarged blood vessels, skin microangiopathy, and various forms of nodules (i.e., rice-grain, pearl- sized or larger-sized nodules in loose connective tissue) are observed during the progression of lipedema in women [41,42,43]. Based on the tissue structure, mobilizing pattern, and pathology, lipedema is characterized by 4 progressive stages.
Stage 1 patients present with a smooth skin texture, an enlarged subdermis, pearl-sized nodules in a hypertrophic SAT layer (which are painful once in a while), and a subdermal pebble-like feel due to underlying LCT fibrosis.
Stage 2 features are skin depressions with pearl to apple-sized masses forming in the skin, palpable nodules, and bands of perilobular fascia that thicken and contract, and inflammatory appearance of the skin (due to progressive fibrotic changes), and pulling down of the skin in matt ress pattern (due to excess tissue).
Stage3 feature more painful, increased lipedema tissue that is more fibrotic in texture with numerous large subdermal nodules and overhanging lobules of tissue, as well as fat on the arms, hips, thighs, around knees and shins. The skin becomes thin and loses elasticity allowing SAT to grow excessively and fold over itself. This inhibits flow of lymph [33] and there could be venous reflux, eventually leading to lipolymphedema or lymphedema.
In stage 4, lipedema is characterized by lipolymphedema (concomitant lymphedema) which develops in the presence of both lipedema and lymphedema, featuring large overhangs of fat tissue on the legs or arms, and large extrusions on the legs that progress to lipolymphedema, thus representing a more advanced stage in most cases [8]. Lipolymphedema (a condition similar to lymphedema) can occur in all stages [44]. This is one of the main reason lipedema is often confused with other metabolic disorders, such as lymphedema, obesity, lipodystrophies, and other fat-related diseases [45].
| Stages of lipedema | |
| Stage 1 | Even skin surface with large hypodermis |
| Stage 2 | Uneven skin pattern, development of nodular subcutaneous nodules, lipomas and/ or angiolipomas |
| Stage 3 | Large growths of nodular fat with severe contour deformity of thighs, around knees and shins. Skin folds develop |
| Stage 4 | All of the above features of stage 3 with lipolymphedema |
Table 1
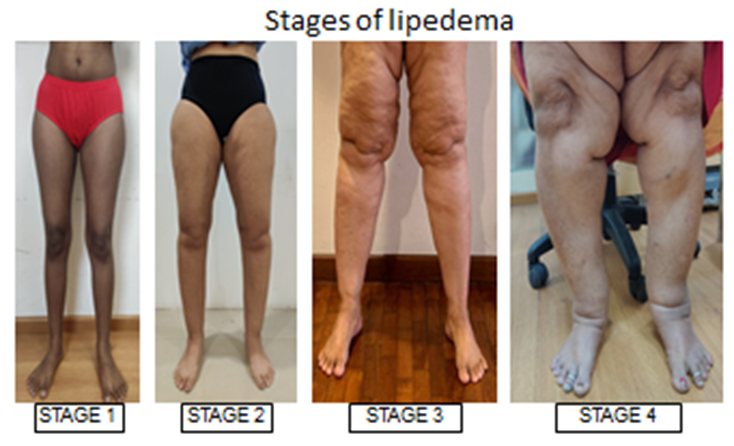
Figure 6: Different stages of lipedema
Types of lipedema:
Based on the pattern of fat distribution and site of involvement, lipedema is classified into 5 different types (2).
Type 1: Unusual increase in size of the hips alone is seen. The thighs and legs are normal.
Type 2: The hips and thighs increase in size abnormally. The legs are not affected.
Type 3: The entire lower body increases in the size abnormally, i.e., the buttocks to ankles. The feet below the ankles are not affected.
Type 4: There is abnormal increase in size of the arms and sometimes the forearms. The hands are spared.
Type 5: There is an abnormal increase in the size of the legs from knees to ankles which appear more cylindrical in the early stages and may have lumpy fat deposits on the upper shin area later. The feet are generally not affected.
The commonest combinations seen are type 2 & 4 and type 3 & 4. Isolated type 5 is uncommon. Only arms may be affected in 30% of lipedema cases [41].
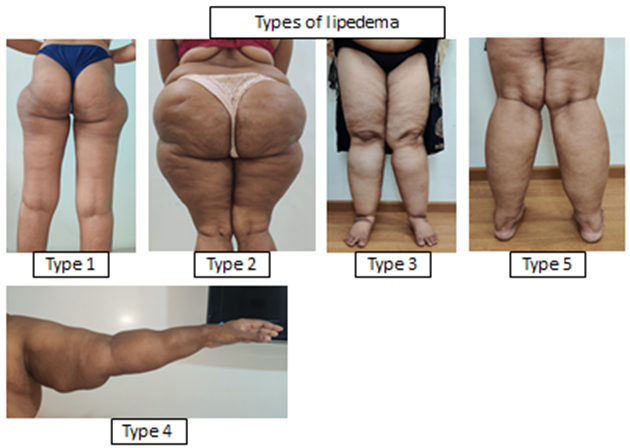
Figure 7: Different types of lipedema based on site of fat distribution
Differential diagnosis of lipedema:
Lipedema has to be clearly distinguished from other entities. Lipedema is often misdiagnosed and differential diagnosis can be challenging.
Benign lipohypertrophy morphologically may resemble lipedema. The most common form being “the riding breeches” obesity where upper extremities are rarely affected [46]. Lipohypertrophy presents without pain, edema or bruising [47] in contrast to lipedema. Though it is not entirely clear that they are separate entities, it is thought that lipedema may develop from lipohypertrophy over time [48].
Primary lymphedema is another differential diagnosis of lipedema which may also affect women around puberty. Lipedema presents with symmetrical swelling while primary lymphedema is usually asymmetrical. While lymphedema starts at the toes first, lipedema starts at the thighs first. One clinical differentiating factor is the Stemmer’s sign which is positive in lymphedema and negative in lipedema [49]. Another significant difference is the presence of pain and frequent bruising in lipedema which is absent in lymphedema. A visible lymphedema can however occur in any stage of lipedema [33].
Dercum’s disease is a condition characterised by generalized obesity and painful fatty tumors in the adipose tissue occurring almost exclusively in women. The tumors are found typically in the extremities without involvement of the feet. It develops around menopause with muscular weakness and fatigue, emotional disturbance, depression and alcohol abuse being potential features [50]. However, there is a controversy whether Dercum’s disease is a separate entity or just a variant of lipedema.
Madelung’s disease, also known as benign symmetrical lipomatosis and Launois-Bensaude disease is a disorder of fat metabolism resulting in unusual accumulation of fat deposits around the neck (type 1), shoulder and upper arms (type2), or pelvis (type 3). The condition is almost exclusively seen in men and is associated with alcohol abuse and liver damage [51].
Phlebolymphedema is the result of chronic venous insufficiency. Typical symptoms are skin discoloration, varicose veins and ulcer formations in the legs. It may occur in men or women and can affect one or both limbs simultaneously. Women with lipedema having varicose veins may develop phlebolymphedema [48]. Ultrasound examination in phlebolymphedema shows pathologic changes.
Lipedema is frequently misdiagnosed as obesity. While lipedema usually affects the lower and/ or upper limbs not affecting the feet and hands, obesity can affect the whole body. There is minimal response to diet and exercise in chronic lipedema patients which can be frustrating because there is less weight reduction in the limbs compared to trunk [52]. There is little response in lipedema affected areas even after extreme weight loss measures like bariatric
| Disease | Lipedema | Lipohypertrophy | Obesity | Lymphedema | Dercum’s | Madelung’s | Phebolymphedema |
| Age of onset | Puberty | Puberty | Any age | Any age | Menopause | Middle age | Any age |
| Gender | Women | Women | Men/ women | Men/ women | Women | Men | Men/ women |
| Fat distribution | Lower/ upper extremities | Lower extremities | Generalized | Extremities | Extremities | Neck, shoulder, arms | Lower limbs |
| Place of origin | Hips/ thighs | Riding breeches | Generalized | Feet | Extremities | Neck, shoulder, arms | One or both limbs |
| Pain | May be present | No | No | No | Yes | Yes | Yes |
| Bruising | Yes | No | No | No | Maybe | No | No |
| Spider veins | Yes | No | No | No | No | No | No |
| Stemmer’s sign | -ve | -ve | +ve/ -ve | +ve | -ve | -ve | -ve |
| Substance abuse | No | No | No | No | Alcohol | Alcohol | No |
surgery. The hallmark of symmetrical fat increase is shared by lipedema and obesity [53]. There is a risk of progression into lipedema in women who cannot have a sustained weight loss. This seems more likely in women experiencing periods of weight loss followed by periods of weight gain [43]. Bariatric surgery may be a successful way of maintaining non lipedema weight loss [54].
Table 2: Differential diagnosis of lipedema
Pathogenesis:
The cause for lipedema is still largely unexplained. It may be in order to understand what we know so far while searching for the unknown. There is an occurrence of both adipose hypertrophy and hyperplasia which results in initial swelling in lipedema [55]. The lymphatic system seems to be functioning normally in the early stages inspite of increased interstitial fluid [56]. In the presence of increased interstitial fluid there is thickening of the interstitium secondary to elevated hydrostatic pressure, in addition to enlarged adipocytes [57,58]. The edema appears to be due to overwhelming of the lymphatic pump rather than a true dysfunction within the lymphatic system. In progressing lipedema, the lymphatic channels stretch and dilate resulting in microaneurysms which have a tendency to leak. The leaking microaneurysms and increased interstitial fluid results in late stage lipolymphedema [56,59,60,61] which results in capillary fragility and leakage corresponding to easy bruising and telengiectasis seen in lipedema patients [62,63]. In addition there appears to be an influx of inflammatory cells within the interstitium contributing to adipocyte hypertrophy [9].
Management:
Treatment options for lipedema are limited presently due to incomplete understanding of the pathophysiology, there are many unanswered questions regarding optimal therapeutic management [64,65]. Understanding patient expectations, available treatment options and tailoring to suit the needs of the patient to provide relief is an essential part of lipedema management. While patients are initially relieved to receive an accurate diagnosis of their condition, it is imperative to provide available solutions to minimize disappointment and psychological distress.
The aims of lipedema treatment are to identify the disease early and reduce lower extremity symptoms and functional limitations while preventing or arresting the progression of the disease. An etiology based treatment for lipedema is presently unavailable and so effective treatment should also target factors that negatively impact lipedema such as obesity, presence of venous or lymphatic edema, decreased physical activity and incorrect insight into the disease [66,67].
Conservative therapies
As lipedema is a chronic, disabling and progressive condition accompanied by extremity pain, loss of strength, deterioration in physical activity and depression, the ultimate goal is to reverse, stall progression or atleast slow the progression. Therapeutic interventions to enable an active lifestyle by improving strength and fitness should be the ultimate goal.
Dietary modifications cannot alter the fat distribution in lipedema patients but can improve prognosis and general well-being. A combination of early weight reduction and diet changes may reduce the local inflammatory changes preventing an exacerbation of lipedema [39,68,69]. Obesity is also an important condition that can be modified for which cooperation with a dietician is necessary[70].
Exercise is known to have a beneficial effect on fat tissue. Fat tissue in lipedema is highly resistant to exercise unlike in obesity [7]. Adipose tissue increase induces macrophage infiltration causing slow systemic infiltration [71,72]. Walking, cycling and aerobics and exercises in water have been found to be effective by reducing strain on the joints and increasing lymph drainage in lipedema patients. Calorie utilization is more with water resistance. However water exercises alone is not useful in weight reduction [73].
The existence of relevant edema component must be determined before initiating treatment. Compression therapy and compression garments may be useful in reducing or controlling edema while it stimulates the arterial, venous and lymphatic flow [74]. Intermittent compression therapy also has been found to be a useful tool in containing edema. However, compression has no role in reducing the growth of fat in lipedema.
Medical management:
Use of medicines in lipedema should focus on reducing tissue edema, inflammation, pain and fibrosis. Diuretics helps in reducing edema but should be used for long as the edema is primarily due to inflammation [75]. Diosmin, a biologically active phenol has been found to improve venous elasticity, reduces microvascular permeability and improves vascular, neuropathic and radicular pain in people with chronic venous disease and can be considered for treatment of lipedema [76,77]. Metformin inhibits hypoxia-induced fibrosis in adipose tissue and should be considered for use in lipedema [78]. Thyroid function should be assessed in women with lipedema. Vitamin D and Selenium are found to be decreased in obese and lipedema and supplementation should be considered.
Reduction in metabolic complications is a beneficial effect following weight reduction in non lipedema obesity [79]. A BMI of greater than 50 kg/m2 can induce metabolic complications, lymphedema and exacerbate lipedema [80].
Surgical management:
Surgical options should be considered for patients who are symptomatic or noticing progressing disease despite conservative measures. Presence of incompetent varicose veins should be assessed and should be treated to reduce the increased incidence of bleeding during liposuction. Care should be taken to protect the lymphatic and venous system at all times. Lipectomy with skin excision can be considered in certain conditions where contour needs to be addressed. The tumescent technique and water assisted liposuction were found to be beneficial in protecting the lymphatic system. Liposuction improves pain, swelling, function, physical appearance and quality of life [25,81,82]. More than two sessions are often required to treat the extremities adequately along its entire length. It is presumed that no new fat cells will be formed after surgery. Limits of safety and cosmetic consequences should be considered while removing as much of fat as is possible to prevent recurrences. The limited remaining fat cells might cause minor visible tissue growth. Following surgery conservative treatment methods can be terminated or reduced in over 65% of treated patients. However, they are necessary occasionally and quality of life, sensitivity and mobility are improved noticeably [21].
Summary:
Lipedema is a common but underdiagnosed and often misdiagnosed entity. Lipedema was recognized by WHO in 2019 as a separate disease entity. An increased awareness about lipedema is essential among clinicians to identify and treat affected lipedema patients effectively. Early detection and treatment should be made to alleviate the symptoms, improve function and quality of life. Conservative therapies like compression bandages, stockings and garments and lymphatic compression pumps are the main pillars for lipedema treatment and complement to improve surgical outcomes. Lymphatic vessel sparing liposuction and occasional excisional lipectomy can be considered for patients not responding well to conservative treatments. Adequate liposuction appears to be the most effective surgical treatment with long term benefits to date. Varicose veins should be addressed timely to avoid associated late complications as necessary.
References
- Kruppa P, Georgiou I, Biermann N, Prantl L, Klein-Weigel P, Ghods M. Lipedema- (2020) Pathogenesis, Diagnosis, and Treatment Options. Dtsch Arztebl Int. 2020 Jun 1;117(22-23):396-403. doi: 10.3238/arztebl.2020.0396. PMID: 32762835; PMCID: PMC7465366.
--> - Buck DW 2nd, Herbst KL. Lipedema: (2016) A Relatively Common Disease with Extremely Common Misconceptions. Plast Reconstr Surg Glob Open. 2016 Sep 28;4(9): e1043. doi: 10.1097/GOX.0000000000001043. PMID: 27757353; PMCID: PMC5055019.
Publisher | Google Scholor - Allen EV, Hines EAJ. Lipedema(1940) of the legs: a syndrome characterised by fat legs and orthostatic edema. Proc Staff Meet Mayo Clin; 15: 184–187.
--> - Moncorps CB, Brinkhaus G, Herteld F, (1940) et al. Experimentelle untersuchungen zur frage akrozyanotischer zustandsbilder. Arch Derm Syph; 186: 209–215.
--> - World Health Organization. International statistical classification of diseases and related health problems (11th Revision) http://id.who.int/icd/entity/1172950828 Accessed 1 July 2019.
Publisher | Google Scholor - Wold LE, Hines EA, Jr, Allen EV. (1951) Lipedema of the legs; a syndrome characterized by fat legs and edema. Ann Intern Med;34:1243–1250. [PubMed] [Google Scholar]
Publisher | Google Scholor - Herbst KL. (2012) Rare adipose disorders (RADs) masquerading as obesity. Acta Pharmacol Sin. Feb;33(2):155-72. doi: 10.1038/aps.2011.153. PMID: 22301856; PMCID: PMC4010336.
--> - Buso G, Depairon M, Tomson D, (2019) et al. Lipedema: a call to action! Obesity (Silver Spring) 27: 1567–1576.
Publisher | Google Scholor - Földi M, Földi E, Strößenreuther R, Kubik S. (2012) Urban & Fischer. München, Germany: Lipedema Földi‘s textbook of lymphology: for physicians and lymphedema therapists 3rd Edition; pp. 364–369. [Google Scholar] [Ref list]
Publisher | Google Scholor - Herpertz U. (1997) Krankheitsspektrum des Lipödems an einer Lymphologischen Fachklinik - Erscheinungsformen, Mischbilder und Behandlungsmöglichkeiten. Vasomed.6:301–307. [Google Scholar] [Ref list]
Publisher | Google Scholor - Meier-Vollrath I, Schneider W, Schmeller W. (2005) Lipödem: Verbesserte Lebensqualität durch Therapiekombination. Dtsch Ärzteblatt.102: A1061–A1067. [Google Scholar] [Ref list]
Publisher | Google Scholor - Microlymphatic aneurysms in patients with lipedema. Amann-Vesti Amann-Vesti, BR BR, Franzeck UK, Bollinger (2001) A. https://journals.uair.arizona.edu/index.php/lymph/article/view/17310. Lymphology.34:170–175. [PubMed] [Google Scholar] [Ref list]
Publisher | Google Scholor - Fluorescence microlymphography: diagnostic potential in lymphedema and basis for the measurement of lymphatic pressure and flow velocity. Bollinger A, Amann-Vesti BR. (2007) https://journals.uair.arizona.edu/index.php/lymph/article/view/17133. Lymphology; 40:52–62. [PubMed] [Google Scholar] [Ref list]
Publisher | Google Scholor - Dilated blood and lymphatic microvessels, angiogenesis, increased macrophages, and adipocyte hypertrophy in lipedema thigh skin and fat tissue. Al-Ghadban S, Cromer W, Allen M, Ussery C, Badowski M, Harris D, Herbst KL. J Obes.2019:8747461. [PMC free article] [PubMed] [Google Scholar] [Ref list]
Publisher | Google Scholor - Uncovering lymphatic transport abnormalities in patients with primary lipedema. Gould DJ, El-Sabawi B, Goel P, Badash I, Colletti P, Patel KM. J Reconstr Microsurg. 2020; 36:136–141. [PubMed] [Google Scholar] [Ref list]
Publisher | Google Scholor - Allen, M.; Schwartz, M.; Herbst, K.L. (2020) Interstitial Fluid in Lipedema and Control Skin. Women’s Health Rep, 1, 480–487. [Google Scholar] [CrossRef]
Publisher | Google Scholor - La Torre, Y.S.-D.; Wadeea, R.; Rosas, V.; Herbst, K.L. Lipedema(2018) Friend and Foe. Horm. Mol. Biol. Clin. Investig. , 33, 1. [Google Scholar] [CrossRef] [PubMed]
Publisher | Google Scholor - L’Hermitte F, Behar A, Paries J, Cohen-Boulakia F, Attali JR, Valensi P. (2003) Impairment of lymphatic function in women with gynoid adiposity and swelling syndrome. Metabolism.52:805–9. [PubMed] [Google Scholar] [Ref list]
Publisher | Google Scholor - Lipedema: is aesthetic cellulite an aggravating factor for limb perimeter? Pereira de Godoy JM, Barufi S, Guerreiro Godoy MF. J Cutan Aesthet Surg. 2013; 6:167–168. [PMC free article] [PubMed] [Google Scholar] [Ref list]
Publisher | Google Scholor - Lipedema: is aesthetic cellulite an aggravating factor for limb perimeter? Pereira de Godoy JM, Barufi S, Guerreiro Godoy MF. J Cutan Aesthet Surg. 2013; 6:167–168. [PMC free article] [PubMed] [Google Scholar] [Ref list]
Publisher | Google Scholor - Peled AW, Kappos EA. Lipedema(2016) diagnostic and management challenges. Int J Womens Health.8:389–395. [PMC free article] [PubMed] [Google Scholar] [Ref list]
--> - Wold LE, Hines EA Jr., Allen EV. (1951) Lipedema of the legs; a syndrome characterized by fat legs and edema. Ann Intern Med;34:1243–1250. [PubMed] [Google Scholar] [Ref list]
Publisher | Google Scholor - Chen SG, Hsu SD, Chen TM, Wang HJ. (2004) Painful fat syndrome in a male patient. Br J Plast Surg; 57:282–286. [PubMed] [Google Scholar] [Ref list]
Publisher | Google Scholor - Czerwińska M, Ostrowska P, Hansdorfer-Korzon R. Lipoedema (2021) as a Social Problem. A Scoping Review. Int J Environ Res Public Health. 2021 Sep 28;18(19):10223. doi: 10.3390/ijerph181910223. PMID: 34639524; PMCID: PMC8508106.
Publisher | Google Scholor - Forner-Cordero, I, G Szolnoky, A Forner-Cordero, et al: Lipedema(2012): An overview of its clinical manifestations, diagnosis and treatment of the disproportional fatty deposition syndrome-systematic review. Clin. Obesity 2, 86-95
Publisher | Google Scholor - Vyas A, Adnan G. Lipedema. [Updated 2022 Sep 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK573066/
--> - Fatima L.A., Campello R.S., Santos R.S., Freitas H.S., Frank A.P., Machado U.F., Clegg D.J. (2017) Estrogen receptor 1 (ESR1) regulates VEGFA in adipose tissue. Sci. Rep.7:16716. doi: 10.1038/s41598-017-16686-7. [PMC free article] [PubMed] [CrossRef] [Google Scholar] [Ref list]
Publisher | Google Scholor - Holmes D.I., Zachary I. (2005) The vascular endothelial growth factor (VEGF) family: Angiogenic factors in health and disease. Genome Biol; 6:209. doi: 10.1186/gb-2005-6-2-209. [PMC free article] [PubMed] [CrossRef] [Google Scholar] [Ref list]
Publisher | Google Scholor - Applanat M.P., Buteau-Lozano H., Herve M.A., Corpet A. (2008) Vascular endothelial growth factor is a target gene for estrogen receptor and contributes to breast cancer progression. Adv. Exp. Med. Biol ;617:437–444. doi: 10.1007/978-0-387-69080-3_42. [PubMed] [CrossRef] [Google Scholar] [Ref list]
Publisher | Google Scholor - Garvin S., Nilsson U.W., Huss F.R., Kratz G., Dabrosin C. (2006) Estradiol increases VEGF in human breast studied by whole-tissue culture. Cell Tissue Res. ;325:245–251. doi: 10.1007/s00441-006-0159-7. [PubMed] [CrossRef] [Google Scholar] [Ref list]
Publisher | Google Scholor - Katzer K, Hill JL, McIver KB, Foster MT. (2021) Lipedema and the Potential Role of Estrogen in Excessive Adipose Tissue Accumulation. Int J Mol Sci. 2021 Oct 29;22(21):11720. doi: 10.3390/ijms222111720. PMID: 34769153; PMCID: PMC8583809.
Publisher | Google Scholor - Beltran K, Herbst KL. (2017) Differentiating lipedema and Dercum's disease. Int J Obes (Lond.); 41: 240–245
Publisher | Google Scholor - Herbst, K.L.; Mirkovskaya, L.; Bharhagava, A.; Chava, Y.; Te, C. (2015) Lipedema Fat and Signs and Symptoms of Illness, Increase with Advancing Stage. Arch. Med. 7, 1–8. [Google Scholar]
Publisher | Google Scholor - Paolacci, S.; Precone, V.; Acquaviva, F.; Chiurazzi, P.; Fulcheri, E.; Pinelli, M.; Buffelli, F.; Michelini, S.; Herbst, K.L.; Unfer, V.; et al. (2019) Genetics of lipedema: New perspectives on genetic research and molecular diagnoses. Eur. Rev. Med. Pharmacol. Sci. , 23, 5581–5594. [Google Scholar] [CrossRef] [PubMed]
Publisher | Google Scholor - Rizner, T.L.; Penning, T.M. (2014) Role of aldo-keto reductase family 1 (AKR1) enzymes in human steroid metabolism. Steroids, 79, 49–63. [Google Scholar] [CrossRef] [PubMed][Green Version]
Publisher | Google Scholor - Michelini, S.; Chiurazzi, P.; Marino, V.; Dell’Orco, D.; Manara, E.; Baglivo, M.; Fiorentino, A.; Maltese, P.E.; Pinelli, M.; Herbst, K.L.; Dautaj, A.; Bertelli, M. Aldo-Keto (2020) Reductase 1C1 (AKR1C1) as the First Mutated Gene in a Family with Nonsyndromic Primary Lipedema. Int. J. Mol. Sci. 21, 6264. https://doi.org/10.3390/ijms21176264
Publisher | Google Scholor - Bauer, A.T.; Von Lukowicz, D.; Lossagk, K.; Hopfner, U.; Kirsch, M.; Moog, P.; Bauer, H.; Machens, H.G.; Schmauss, D. Adipose (2019) Stem Cells from Lipedema and Control Adipose Tissue Respond Differently to Adipogenic Stimulation In Vitro. Plast. Reconstr. Surg. , 144, 623–632. [Google Scholar] [CrossRef]
Publisher | Google Scholor - Felmerer, G.; Stylianaki, A.; Hägerling, R.; Wang, A.; Ströbel, P.; Hollmén, M.; Lindenblatt, N.; Gousopoulos, E. (2020) Adipose Tissue Hypertrophy, an Aberrant Biochemical Profile and Distinct Gene Expression in Lipedema. J. Surg. Res. , 253, 294–303. [Google Scholar] [CrossRef] [PubMed]
Publisher | Google Scholor - Suga, H.; Araki, J.; Aoi, N.; Kato, H.; Higashino, T.; Yoshimura, K. (2009) Adipose Tissue Remodeling in Lipedema: Adipocyte Death and Concurrent Regeneration. J. Cutan. Pathol. 36, 1293–1298. [Google Scholar] [CrossRef]
Publisher | Google Scholor - Ishaq, M.; Bandara, N.; Morgan, S.; Nowell, C.; Mehdi, A.M.; Lyu, R.; McCarthy, D.; Anderson, D.; Creek, D.J.; Achen, M.G.; (2022) et al. Key Signaling Networks Are Dysregulated in Patients with the Adipose Tissue Disorder, Lipedema. Int. J. Obes. , 46, 502–514. [Google Scholar] [CrossRef] [PubMed]
Publisher | Google Scholor - Herbst KL, Kahn LA, Iker E, et al. (2021) Standard of care for lipedema in the United States. Phlebology.;36(10):779-796. doi:10.1177/02683555211015887
Publisher | Google Scholor - Eklof, B.; Perrin, M.; Delis, K.T.; Rutherford, R.B.; (2009) Gloviczki, P. Updated Terminology of Chronic Venous Disorders: The VEIN-TERM Transatlantic Interdisciplinary Consensus Document. J. Vasc. Surg. 49, 498–501. [Google Scholar] [CrossRef]
Publisher | Google Scholor - Wiedner, M.; Aghajanzadeh, D.; Richter, D.F. (2020) Differential Diagnoses and Treatment of Lipedema. Plast. Aesthetic Res. , 7, 10. [Google Scholar] [CrossRef]
Publisher | Google Scholor - Rasmussen, J.C.; Aldrich, M.B.; Fife, C.E.; Herbst, K.L.; Sevick-Muraca, E.M. (2022) Lymphatic Function and Anatomy in Early Stages of Lipedema. Obesity, 30, 1391–1400. [Google Scholar] [CrossRef]
Publisher | Google Scholor - Child, A.H.; Gordon, K.D.; Sharpe, P.; Brice, G.; Ostergaard, P.; Jeffery, S.; Mortimer, P.S. (2010) Lipedema: An Inherited Condition. Am. J. Med. Genet. Part A , 152, 970–976. [Google Scholar] [CrossRef]
Publisher | Google Scholor - Wiedner M, Aghajanzadeh D, Richter DF. (2020) Differential diagnoses and treatment of lipedema. Plastic and Aesthetic Research. ; 7:10. http://dx.doi.org/10.20517/2347-9264.2019.51
Publisher | Google Scholor - Müssig K, Gallwitz B. (2006) Lipohypertrophie. Dtsch Med Wochenschr; 131:1807-8. (in German) PubMed
Publisher | Google Scholor - Herpertz U. (2004) Ödeme und Lymphdrainage. Diagnose und Therapie von Ödemkrankheiten. 2nd ed. Stuttgart, New York: Schattauer;. pp. 168-18122.
Publisher | Google Scholor - Stemmer R. (1976) Ein klinisches zeichen für früh- und differentialdiagnostik des lymphödems. Vasa; 3:261-2.
--> - DeFranzo AJ, Hall JH, Herring SM. (1990) Adiposis dolorosa (Dercum’s disease): liposuction is an effective form of treatment. Plast Reconstr Surg; 85:289-92.
Publisher | Google Scholor - Ruzicka T, Vieluf D, Landthaler M, Braun-Falco O. (1987) Benign symmetric lipomatosis Lau-nois-Bensaude. Report of ten cases and reviewof the literature. J Am Acad Dermatol; 17:663-74. DOIPubMed
Publisher | Google Scholor - Schmeller W, Meyer-Vollrath I. (2004) Erfolgreiche operative therapie des lipödems mittels liposuktion. Phlebologie; 33:23-9.
Publisher | Google Scholor - Bertsch T, Erbacher G. (2018) Lipoedema - myths and facts Part 3. Phlebologie; 47:188-97.
Publisher | Google Scholor - Bertsch T, Erbacher G., Torio-Padron N. (2019) Lipoedema - myths and facts Part 4. Phlebologie; 48:47-56.
Publisher | Google Scholor - van Geest AJ, Esten SCAM, Cambier J-PRA, (2003) et al. Lymphatic disturbances in lipoedema. Phlebologie; 32:138142.
Publisher | Google Scholor - Amann-Vesti BR, Franzeck UK, Bollinger A. (2001) Microlymphatic aneurysms in patients with lipedema. Lymphology; 34:170175.
Publisher | Google Scholor - Stallworth JM, Hennigar GR, Jonsson HT Jr, et al. (1974) The chronically swollen painful extremity. A detailed study for possible etiological factors. JAMA; 228:16561659.
Publisher | Google Scholor - Harwood CA, Bull RH, Evans J, et al. (1996) Lymphatic and venous function in lipoedema. Br J Dermatol.;134:16.
Publisher | Google Scholor - Partsch H, Stöberl C, Urbanek A, et al. (1988) Clinical use of indirect lymphography in different forms of leg edema. Lymphology; 21:152160.
Publisher | Google Scholor - Bräutigam P, Földi E, Schaiper I, et al.(1998) Analysis of lymphatic drainage in various forms of leg edema using two compartment lymphoscintigraphy. Lymphology; 31:4355.
Publisher | Google Scholor - Bilancini S, Lucchi M, Tucci S, et al. (1995) Functional lymphatic alterations in patients suffering from lipedema. Angiology; 46:333339.
Publisher | Google Scholor - Curri SB, Merlen JF. (1986) [Microvascular disorders of adipose tissue]. J Mal Vasc.;11:303309.
Publisher | Google Scholor - https://europepmc.org/article/med/3772261
Publisher | Google Scholor - SugaHArakiJAoiNKatoHHigashinoTYoshimuraKAdipose tissue remodeling in lipedema: adipocyte death and concurrent regenerationJ Cutan Pathol200936121293129819281484 [Crossref], [Web of Science ®], [Google Scholar]
--> - SzélEKeményLGromaGSzolnokyGPathophysiological dilemmas of lipedemaMed Hypotheses201483559960625200646 [Crossref], [Web of Science ®], [Google Scholar]
--> - Dutch Society for Dermatology and Venereology and the Dutch Academy of Medical SpecialistsLipedema Guidelines in the Netherlands 2014UtrechtDutch Society for Dermatology and Venereology2014 [Google Scholar]
--> - GoodliffeJMOrmerodJOBealeARamcharitarSAn under-diagnosed cause of leg swellingBMJ Case RepEpub2013524 [Crossref], [Google Scholar]
--> - Reich-Schupke S, Altmeyer P, Stücker M. (2013) Thick legs – not always lipedema. J Dtsch Dermatol Ges.;11(3):225–233. [PubMed] [Google Scholar]
Publisher | Google Scholor - Damstra RJ, Andrade M, Villavicencio JL. (2013) Diagnosis and treatment of primary lymphedema. Consensus document of the International Union of Phlebology (IUP)-2013. Int Angiol.;32(6):541–574. [PubMed] [Google Scholar]
Publisher | Google Scholor - Langendoen SI, Habbema L, Nijsten TE, Neumann HA. (2009) Lipoedema: from clinical presentation to therapy. A review of the literature. Br J Dermatol.;161(5):980–986. [PubMed] [Google Scholar]
Publisher | Google Scholor - Yudkin, J (2007) Inflammation, obesity, and the metabolic syndrome. Horm. Metab. Res. 39, 707-709.
Publisher | Google Scholor - Handschin, C, BM Spiegelman: (2008) The role of exercise and PGC1α in inflammation and chronic disease. Nature 454, 463.
Publisher | Google Scholor - Weiner, R: (2015) Adipositas-Wann ist der Chirurg gefragt? DMW-Deutsche Medizinische Wochenschrift 140, 29-33.
Publisher | Google Scholor - Damstra RJ, Andrade M, Villavicencio JL. (2013) Diagnosis and treatment of primary lymphedema. Consensus document of the International Union of Phlebology (IUP)-2013. Int Angiol.;32(6):541–574. [PubMed] [Google Scholar]
Publisher | Google Scholor - Felmerer G, Stylianaki A, Hägerling R, et al. (2020) Adipose tissue hypertrophy, an aberrant biochemical profile and distinct gene expression in lipedema. J Surg Res; 253: 294–303.
Publisher | Google Scholor - Ibegbuna V, Nicolaides AN, Sowade O, et al. (1997) Venous elasticity after treatment with Daflon 500 mg. Angiology; 48: 45–49
Publisher | Google Scholor - Batchvarov IV, Batselova MG, Damyanov II. (2010) min therapy (600 mg) in patients with chronic venous insufficiency—results and analysis. J Biomed Clin Res; 3: 51–54.
Publisher | Google Scholor - Li X, Li J, Wang L, et al. (2016) The role of metformin and resveratrol in the prevention of HIF1-alpha accumulation and fibrosis in hypoxic adipose tissue. Br J Pharmacol; 5: 13493.89)
--> - Bays HE, Mw Christensen S, Tondt J, et al. (2020) Obesity algorithm slides. Scarborough: Obesity Medicine Association.
Publisher | Google Scholor - Greene AK, Sudduth CL. (2021) Lower extremity lymphatic function predicted by body mass index: a lymphoscintigraphic study of obesity and lipedema. Int J Obes; 45: 369–373.
Publisher | Google Scholor - DudekJEBiałaszekWOstaszewskiP. Quality of life in women with lipoedema: a contextual behavioral approachQual Life Res201625240140826216585 [Crossref], [Web of Science ®], [Google Scholar]
--> - Warren PeledA, SlavinSA, BrorsonH. Long-term outcome after surgical treatment of lipedema Ann Plast Surg201268330330721629090 [Crossref], [Web of Science ®], [Google Scholar]
-->
 Alcrut
Alcrut