Case report
- Mohamed Ali Gliti*
- Niema Benkhraba
- Zainab Benyahia
- Razika Bencheikh
- Mohamed Anas Benbouzid
- Abdelilah Oujilal
- Leila Essakalli Houssyni
ENT Department, Rabat Specially Hospital, Ibn Sina University Hospital, Hafiane-cherkaoui Avenue, 10100 Rabat, Morocco
1 Resident physician in otolaryngology, Department of Otolaryngology, Head and Neck Surgery, Ibn Sina University Hospital, Rabat, Morocco
2 Professor of otolaryngology, Department of Otolaryngology, Head and Neck Surgery, Ibn Sina University Hospital, Rabat, Morocco
3 Faculty of Medicine and Pharmacy of Rabat, Mohamed V University, Rabat, Morocco
*Corresponding Author: Mohamed Ali Gliti
Citation: Mohamed Ali Gliti, Niema Benkhraba, Zainab Benyahia, Razika Bencheikh, Mohamed Anas Benbouzid, Abdelilah Oujilal, Leila Essakalli Houssyni, Isolated Sphenoidal Aspergillosis: Case report and review of literature, J Journal of Clinical and Medical Case Reports and Reviews V(2)I(3).
Copyright: © 2022 Mohamed Ali Gliti, This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in
Received: November 05, 2022 | Accepted: November 26, 2022 | Published: November 29, 2022
Abstract
Sphenoidal aspergillosis is a rare condition whose diagnosis is not always obvious. The clinician should always bear this diagnosis in mind in patients with chronic sinusitis avoiding invasive and fulminant forms which could be life-threatening. In fact, this work focused on the description of the clinical features of this entity as well as its management by presenting a case report and reviewing literature.
Keywords: sphenoidal sinus, Aspergillosis, Endoscopic sphenoidotomy.
Introduction
Sphenoidal aspergillosis is a rare disease whose incidence is estimated at 1.2 % per year [1]. This incidence has undergone an increase in the last decade, due to an epidemiological shift towards fungal infections, and this, in front of the use of antibiotics, corticosteroids, and the development of diagnostic means [2]. Besides, this entity could be probably underestimated due to the lack of systematic mycological sampling and anatomopathological study [3].
Mycotic infection is serious, fatal and its prognosis depends closely on the treatment delay. Diagnosis is usually delayed in the absence of specific clinical signs. Clinician must keep this rare entity in mind, in order to avoid the progression into invasive forms, prognosis of this latest is poorer even with a fatal outcome, and since surgery won't be curable, thus urgent antifungal treatment will be required.
Case report
This is a 72-year-old patient, who for several years had chronic headaches, most often on the right, associated with posterior purulent rhinorrhea. The sinus CT scan showed an opacity of the right sphenoid sinus suggestive of aspergillosis (Figure 1). The patient benefited from endoscopic sphenoidotmia with evacuation of purulent intrasinus contents and excision of the pathological mucosa (Figure 2). The pathological study confirms the diagnosis of aspergillosis. The postoperative results were good.
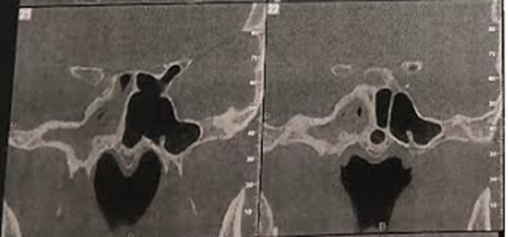
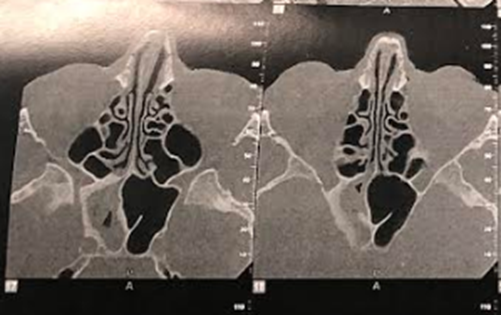
Figure 1: Sinus CT scan (Coronal and axial image) showing opacity of the right sphenoidal sinus.

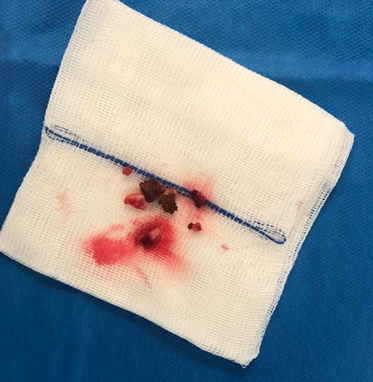
Figure 2: A Peroperative image, B Bacteriological samples (Aspergiloma)
Discussion
Aspergillosis is known as a fungal infection caused by a ubiquitous germ of the genus Aspergillus with a prevalence of fumigatus and flavus species [5]; Aspergillosis commonly involve the maxillary and frontal sinuses. The sphenoidal site, however, is exceptional [3].
Different forms of sphenoidal aspergillosis were described: the noninvasive form, the invasive form that includes chronic invasive sinusitis and fulminant sinusitis that may have serious consequences [6].
Typically, fungal sphenoid sinusitis occurs in immunocompromised subjects and without having any nasal complaints. In fact, cases of sphenoid sinus fungal infection, reported in the literature, without immunocompromise are very common [7], and seems to be related to the chronic noninvasive forms described in the current investigation.
On the other hand, many authors have identified a set of risk factors and predisposing medical disease which associated to developing sphenoid aspergillosis more than others, such as patients having allergy, alcoholism, long-term corticosteroid therapy, diabetes, AIDS, the use of anti-tuberculosis drugs or following solid organ transplantation [2,3]. Hypercoticism also has been associated with an increased incidence of aspergillosis [3].
Usually the complications are inaugural of the infection when the invasion hits the structures adjacent to the sinus. The clinical presentation can be neurological, rhinological or even ophthalmological.
The sphenoidal location of aspergillosis and the proximity of the neuro-vascular structures are a source of ophthalmological and endocranial complications. These phenomena are explained by mycelial growth and production of cytotoxic metabolites responsible for soft tissue and bone destruction [6].
Intracranial complications involve skull base osteomyelitis, meningitis, meningoencephalitis, brain abscess, and cavernous sinus thrombosis, involvement of orbital apex, infarcts, and rarely mycotic anevrysm [7].
Starting with neurological signs, headache represents one of the most common signs of sphenoidal aspergillosis reported between 67% and 85
Conclusion
Chronic noninvasive sphenoid sinus aspergillosis appears to be a benign disease, essentially affecting women and patients over the age of 50 years. Symptoms are fairly non-specific. Imaging and histological examination are essential for management. The invasive form is a serious disease requiring rapid, multidisciplinary management.
References
- Thery A., Espitalier F., Cassagnau E., Durand N., Malard O. Clinical features and outcome of sphenoid sinus aspergillosis: a retrospective series of 15 cases. Eur. Ann. Otorhinolaryngol. Head Neck Dis. août 2012;129(4):179–184. doi: 10.1016/j.anorl.2011.06.005.
Publisher | Google Scholor - Kamaoui I., et al. Aspergillose sphénoïdale révélée par des signes neuro-ophtalmologiques: à propos d’un cas. J. Radiol. juin 2007;88(6):901–903. doi: 10.1016/S0221-0363(07)89893-3.
Publisher | Google Scholor - Zainine R., Hachicha A., Gamra S.B., Beltaief N., Sahtout S., Besbes G. Aspergillose sphénoïdale chez deux patients immunocompétents. J. Mycol. Med. juin 2011;21(2):142–145. doi: 10.1016/j.mycmed.2011.03.006. [CrossRef]
Publisher | Google Scholor - Agha R.A., et al. The SCARE 2020 guideline: updating Consensus Surgical CAse REport (SCARE) Guidelines. Int. J. Surg. déc. 2020; 84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [Abstract] [CrossRef] [Google Scholar]
Publisher | Google Scholor - Shams M.G., Motamedi M.H.K. Aspergilloma of the maxillary sinus complicating an oroantral fistula. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. juill. 2003;96(1):3–5. doi: 10.1016/S1079-2104(03)00006-4. [Abstract] [CrossRef]
Publisher | Google Scholor - A. Devèze, F. Facon, G. Latil, G. Moulin, H. Payan-Cassin, P. Dessi, Cavernous Sinus Thrombosis Secondary to Non-invasive Sphenoid Aspergillosis, p. 5. 2005. [Abstract]
Publisher | Google Scholor - Jain A., Goyal K., Meher R., Passey J.C. Internal carotid artery bleed: a rare complication of invasive sphenoidal aspergillosis. World Neurosurg. sept. 2019; 129:292–294. doi: 10.1016/j.wneu.2019.06.014. [Abstract] [CrossRef]
Publisher | Google Scholor - Chopra H., Dua K., Malhotra V., Gupta R.P., Puri H. Invasive fungal sinusitis of isolated sphenoid sinus in immunocompetent subjects. Mycoses. janv. 2006;49(1):30–36. doi: 10.1111/j.1439-0507.2005.01170.x. [Abstract]
Publisher | Google Scholor - Lee D.H., Yoon T.M., Lee J.K., Joo Y.E., Park K.H., Lim S.C. Invasive fungal sinusitis of the sphenoid sinus. Clin. Exp. Otorhinolaryngol. 2014;7(3):181. doi: 10.3342/ceo.2014.7.3.181. [Europe PMC free article] [Abstract]
Publisher | Google Scholor - Boutarbouch M., Arkha Y., El Ouahabi A., Derraz S., El Khamlichi A. Sphenoid sinus aspergillosis simulating pituitary tumor in immunocompetent patient. J. Clin. Neurosci. juin 2009;16(6):840–841. doi: 10.1016/j.jocn.2008.08.032. [Abstract] [CrossRef]
Publisher | Google Scholor - Aribandi M., McCoy V.A., Bazan C. Imaging features of invasive and noninvasive fungal sinusitis: a review. RadioGraphics. sept. 2007;27(5):1283–1296. doi: 10.1148/rg.275065189. [Abstract] [CrossRef]
Publisher | Google Scholor - . Klossek J.-M., Kauffman-Lacroix C., Dufour X. Agent fongique et pathologie rhinosinusienne. Rev. Fr. Allergologie Immunol. Clin. janv. 2005;45(1):25–28. doi: 10.1016/j.allerg.2004.10.011. [CrossRef]
Publisher | Google Scholor - Baumann A., Zimmerli S., Häusler R., Caversaccio M. Invasive sphenoidal aspergillosis: successful treatment with sphenoidotomy and voriconazole. ORL. 2007;69(2):121–126. doi: 10.1159/000097858. [Abstract] [CrossRef]
Publisher | Google Scholor - Klastersky J. Empirical antifungal therapy. Int. J. Antimicrob. Agents. févr. 2004;23(2):105–112. doi: 10.1016/j.ijantimicag.2003.11.002. [Abstract] [CrossRef]
Publisher | Google Scholor - Denning D.W., et al. Efficacy and safety of voriconazole in the treatment of acute invasive aspergillosis. Clin. Infect. Dis. mars 2002;34(5):563–571. doi: 10.1086/324620. [Abstract] [CrossRef]
Publisher | Google Scholor
 Alcrut
Alcrut